LON is now used in our center only in cases of unilateral femoral or tibial lengthening after appropriate counselling , when purely internal methods are excluded because of financial and funding limitations.
LON was introduced as an idea to reduce the time spent on an external fixator and the related problems. External fixation is safe, but the consolidation phase tends to take too long. The prolonged fixator time puts the patience of the patient to the test and, when applied to the femur, this prolonged duration tends to increase knee stiffness.
Moreover, eccentric loading of bones in the limb creates a tendency for axial deviation of the regenerate and malunion. Loosening of the fixation pins, instability of the fixator and tightness of muscles increase the tendency for axial deviation in the lengthening phase.
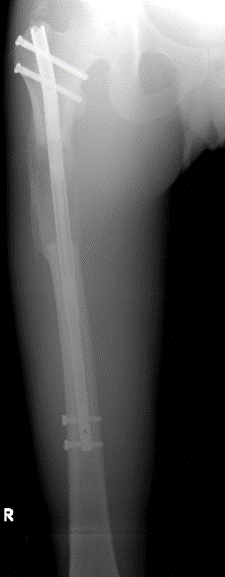
Combining IM fixation with the Ilizarov fixator firstly adds to the stability of the construct. The next benefit of the addition of the IM nail is the prevention of axial deviation during the fixation period and also after removal of the fixator over the long term. This was proved in our series with very low rates of axial deviation.
The greatest concern with LON technique has been the risk of deep bone infection due to close proximity of external pins and the nail. With great care in pin insertion and postoperative care we have not faced this problem in our series. However, the literature has mentioned this problem in the series of Simpson who had three deep infections in twenty LON surgeries. Kristiansen reported giving up on this method to revert back to the Ilizarov technique due to many complications.
The surgical technique of the LON procedure include:
- Preparation (drilling holes) of the osteotomy site.
- Completion of reaming of the intrmedullary canal (to prepare it for the nail).
- Partial application of the external frame (with reamer insitu as a reference to guide external pins and wires clear from the nail.)
- Completion of osteotomy.
- Insertion of the nail and proximal locking only.
- Completion of external frame construct as needed
When the distraction phase is completed, the patient is taken back to theatre where the nail is locked distally with to screws and the external frame is removed. This is a minor procedure which is done as a day case and the patient leaves the hospital on the same day.

 of the PRECICE proprietary technology.
of the PRECICE proprietary technology.
